|
Receding gums can be scary, even uncomfortable. It is important to know that there are a number of factors that can cause your gums to recede. Let’s try to understand why it happens and what you can do about it. Causes:Once it was thought it is inevitable to get “long in the tooth”. However this is far from the truth. It is a disease process, and indicates a current or prior periodontal (gum) disease. Teeth are designed to last a lifetime, with attention to proper oral hygiene, diet and dental care — they should. Let’s start with what’s normal. In a healthy situation teeth erupt into the mouth with the roots fully centered in, and surrounded by jawbone. The gum tissues behave almost like an investing curtain covering the bone; they surround the necks of the teeth like the collar of a turtleneck sweater. In addition to periodontal disease caused by dental (bacterial) plaque, the three most common factors that contribute to gum recession are: the position of your teeth, your genetics, and trauma. Tooth Position. If a tooth erupts in a position that is not aligned within the dental arch, this means thinner bone covering one side of the tooth. Thin bone usually end up with receding gum line. This is also important when moving teeth with braces. Tooth movement via braces will cause bone resorption that will be followed by gum recession. Genetics. Gum texture is genetic. Some types of gums are thin and prone to receding easier than thick gums. Trauma. This happens with overzealous brushing, using too rough a toothbrush, or using a bad technique with scrubbing instead of gently brushing. Periodontal disease. Once a layer of bacteria is formed on the tooth structure, the germs start attacking the tissues including the gums and later on the bone if they access to it. Management:The recession as such can be treated by surgery, where the gum is pulled to cover the exposed tooth. However, the underlying cause needs to be determined before treating the recession. If the cause is not managed, any treatment will fail and the gums will reced again. Conclusion:Prevention of gum recession is very important. Treating a receding gum can be difficult. Make sure you use the right brush and use it properly.
0 Comments
Sometime teeth do not end up with any contact between them, when this happens between op front teeth it is called midline diastema. We are talking about the cases where such space is not created by decay or tooth loss. The cause for this space is general what is called a freenum (pronounced “free – num”, or frenulum (fren-u-lum). This is a fold of tissue that connects the gum to the lip and sometimes contains muscle tissue. If it is unusually large it may connect through to the gum tissue between the teeth and extend to the front portion of the roof of your mouth, or palate. Sometimes, the frenum attachment extends lower than usual and contributes to a separation of the front teeth, and may contribute to keeping them apart. If any teeth alignment is anticipated with orthodontic treatment, then the frenum is better removed, because it might cause the space to re-appear. Removal of the frenum is called a “frenectomy.” Other causes for spacing between front teeth: 1- deep bite (excessive overlap of upper and lower front teeth). 2- tongue thrust (from an involuntary tongue habit). 3- habits, loike tongue or finger sucking. 4- supernumerary, extra tooth that might develop in the midline and does not erupt. The orthodontist can then direct the proper treatment to close the space between the front teeth and decide whether it can be closed by simple movement requiring no more than a retainer, or whether more complex movement is necessary requiring braces. The orthodontist will also decide upon the timing of the frenectomy and whether additional retention will be necessary, such as use of a removable retainer or fixed retainer to stop the teeth from moving apart again. It is generally better to close the space between the front teeth before removing the frenum, because prior removal can result in scar tissue that can prevent space closure. It is also not a good idea to have surgery before the teeth are moved, because it can leave a “black” triangular hole if too much tissue is taken away; it is also difficult to gauge how much tissue to remove before the teeth are moved into correct position. Frenectomy is generally an uneventful, small and limited surgical procedure. It is easily accomplished in the right hands, carried out by a periodontist (gum specialist), oral surgeon, or dentist with surgical training. It is performed by locally anesthetizing (numbing) the area and then dissecting out or undermining the frenum tissue, leaving a very small wound, which is usually completely closed with a few stitches. This can either be accomplished with a small scalpel or with a special dental laser, which “paints away” the unwanted tissue leaving only a small wound with minimal discomfort. In either case healing is usually rapid and uneventful and usually complete in a week or so. Any discomfort should be manageable with no more than non-steroidal anti-inflammatory pain killing medication like aspirin or ibuprofen and antibacterial saltwater mouth-rinses. If orthodontic treatment is not recommended or not considered an option, the gap can be closed by cosmetic restorative work, like direct veneers, porcelain veneers or crowns. Conclusion:Space between top front teeth can be managed, either by orthodontics, surgery, or restorative work. If the cause is a frenum, it must be removed.
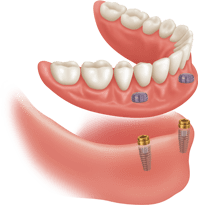
One of the easiest way and most comfortable to have a stable lower denture is by using overdentures. With this treatment, the overdenture rests directly on your gums and is retained by implants placed into your jaw. The overdenture, which is removable, is secured to your implants through retentive attachments incorporated into the denture. Implant-retained tissue supported dentures are currently recognized as the minimum standard of care for fully edentulous patients. Benefits of overdentures Promotes better digestion:Poor fitting dentures are often held in by using adhesives. Overdentures utilize dental implants, so they are more stable than adhesives. Improved stability allows you to chew food more thoroughly, helping your stomach break down food more efficiently, and absorb more nutrients. Slows bone loss by stimulating the bone in your jaw:The overdenture will continue to stimulate your jaw bone when you eat. This stimulation will slow or even stop the resorption (shrinkage) process that is natural when teeth are missing. Helps retain your facial features and structure:The natural process of resorption (shrinkage) that occurs when you have an unhealthy or under-stimulated jaw as a result of missing teeth can, throughout time, cause the distance between your nose and your chin to shrink. This shrinking can make your face look “sunken-in” and prematurely aged. Improved comfort:When your overdenture is retained with implants it fits more securely than one held in with only adhesives. This fit also increases the stability of the overdenture reducing or even eliminating, unnecessary movement during chewing and talking. This lessens the instances of sores and embarrassing dislodgement. Conclusion:If you have dentures or need one, do not settle for less than implant-retained overdenture. Get the best value for money you can have.
What do we mean by simple? In this context simple as opposed to painful. Many people think that having an implant is just a painful dental procedure. However, the procedure is not painful. It is done under local anesthesia, and it does not involve drilling as such, but gently preparing the jaw bone for the implant. What does that mean? This means that if you need an implant or were advised of having one, the most important factor making you refrain from proceeding is fear of pain. The reality: Implant procedure is not painful at all. On the day of the procedure, everything is done under local anesthesia, so just like having a filling, you will not feel a thing. After the numbing wears off, some discomfort is expected. If the procedure involved lots of bone trimming – which is not that common at all – some pain might develop, but this pain is easily managed with some pain killers, it is not a toothache. Conclusion:If you are holding back on having an implant because of fear of pain, then rest assured the procedure is not painful. No need to hold back. For a reminder of the steps for an implant, click here
|
AuthorArticles are written by Dr M Hajarat. Archives
July 2024
|
|
Niagara Park Dental
3 / 16 Washington Avenue Niagara Park, NSW 2250 Email: [email protected] Phone: (02) 4329 3003 |
HOURS
Mon 9:00 - 5:30 Tue 9:00 - 5:30 Wed 9:00 - 5:30 Thu 9:00 - 5:30 Fri 9:00 - 5:30 |
|