|
One of the habits we like is nibbling on chocolate treats. We can have them sitting in the lounge room to nibble as we watch TV. Unfortunately, many of these treats can be very bad for your teeth. If you like that habit, try to control it, first try to decrease the size of your rations, what helps is having some water sitting next to your treats, and chances are you won’t get up to brush your teeth, so the least you can do is sip some water, squish it around and drink it. Another idea might be is to have some Xylitol gum after indulging in your treats. Try to find a sugar free option. Indulging in this habit, makes it all more important not to miss your bed time brushing and flossing.
0 Comments
Why are fruits and veggies good for you? Nutrients and antioxidants found in fruits, vegetables, and even nuts strengthen your immunity and improve the body’s ability to fight tooth decay caused by bacteria and inflammation. Best food for your oral health: Vitamin D with calcium, such as milk, dairy products like cheese, and juices. Vitamin D strengthens teeth and bones.
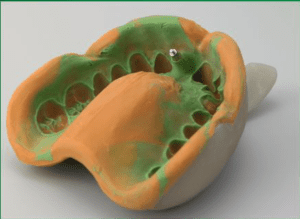
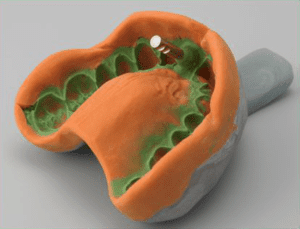
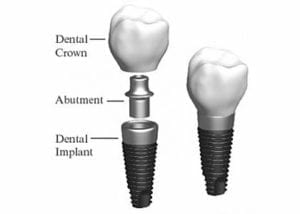
• Vitamin C strengthens the fibres of gums and bones. Like in Citrus fruits and Kiwi fruit. • Folic acid is an important promoter for cellular growth in gums and all over. it is found in green veggies. The frequency and timing of eating is as important as the quality of food. Avoid eating between meal times, avoid sticky food that needs longer to chew. Replacing a tooth with an implant involves many visits and the patient feels the dentist keeps changing pieces, so what exactly is the dentist placing? What are the parts that comprise an implanted tooth? 1- First part is called a fixture, often referred to as the implant as well. It is a piece of titanium rod placed into the jaw bone. It represents the tooth root. It comes packed sterile. The top part of the implant is attached to a “fixture mount” which is used only to carry the fixture from its sterile packaging into the jaw bone. The fixture itself must not touch anything, it goes from the package to bone. The fixture comes in various sizes, varying in width and length. Generally speaking, the standard size for a molar tooth is 4.5mm diameter, with 11mm length. For anterior teeth we can use a 3.5mm diameter, 11mm length. Studies show long term success with smaller implants, but if there is room we try to stick to the bigger implants Once the implant is placed in the jaw, the implant mount is unscrewed from the implant. 2- Now we have a fixture placed in the jaw. The next piece to be used is called gingiva former, or healing cap. It gets screwed into the implant. The function of it, as the name indicates is to force the healing of the gum around the neck of the former, resulting in a tight seal and forming the gums to receive the final crown to mimic natural teeth. The cap is meant to protrude through the gums. The stitches go around it. The patient goes home with the cap showing through. 3- After the implant has deemed to be ready to receive the final restoration, which is between 6 to 12 weeks, the dentist will unscrew the healing cap. An impression is needed to represent the implant, teeth, and tissues, in exact relation to each other. A piece called impression coping is screwed into the implant and an impression is taken. This piece comes out half buried in the impression material. 4- A piece that represents the implant is needed. It is called Implant analogue. It gets screwed to the impression coping. In the meantime, the healing cap is screwed back into the fixture. The impression is sent to the lab to fabricate the final restoration. 5- The lab pours the impression giving him a plaster model, that represents the mouth and the implant. A rubbery material is also used, it replicates the gum around the implant. The technician will choose an abutment of adequate dimensions and angulation. This the next piece required. It is called the definite abutment. The lab uses it first. The technician screws it to the model. He might adjust it by trimming. The lab will fabricate the porcelain crown on tp of the abutment. He sends both the abutment and crown to the dentist.
The dentist first unscrews the healing cap, then screws in the definite abutment, followed by the crown. The crown might be cemented onto the abutment, or screwed onto it. So you decided to go ahead an have a dental implant. Dental implants are used for many scenarios, and in all of these scenarios antibiotics may play a role to ensure good healing. The mouth harbors multiple bacterial species capable of causing infection. Even minimally invasive dental procedures, including dental implant surgery, can allow bacteria to enter the bloodstream. Pre-medicating with antibiotics prior to the surgery can prevent bacteria from reaching and infecting high-risk areas of the body. This is more important for people with high risk conditions. Most people do not fall into this category but if you do (based on your medical history) your doctor will let you know and discuss it with you. Even though dental implants typically have a high rate of survival (over 90%), some may fail due to local bacterial contamination. Infections immediately following surgical implant placement are difficult to treat and almost all infected implants need to be removed. For any structure to stand firm needs to have stable base. The implant is the base that will hold the crowns, so the implant needs to be healthy. High And Low Risk IndividualsOlder adults with a weakened immune system or other serious health problems, smokers, diabetics and those who may be underweight or overweight are especially at risk for infection. The use of prophylactic (preventive) antibiotics is particularly important for patients at high risk for infection. This includes individuals with prosthetic heart valves, a history of infective endocarditis, a heart transplant, and certain congenital (present from birth) heart conditions. Prophylactic antibiotics are no longer routinely recommended for all prosthetic joints. However, some orthopedic surgeons recommend prophylactic antibiotics for patients with artificial joints for up to two years following replacement surgery. Evidence-Based Research FindingsGenerally it is still debated whether clinically healthy, low- and moderate-risk individuals should be prescribed antibiotics for dental implant surgery. The concerns include side effects that range from diarrhea to allergic reactions, and the rise in the appearance of antibiotic-resistant bacteria. A recent study found that taking oral antibiotics before dental implant surgery can be beneficial. It reported that 2 grams of amoxicillin given as a single dose an hour before surgery may reduce implant failure in ordinary conditions without any significant adverse outcomes. The reviewers also inferred that giving antibiotics to 25 people would avoid one person experiencing early implant loss. They did not find any clear evidence about the benefit of taking antibiotics after surgery, or which antibiotics work best. Conclusion:A dose of antibiotics before the surgery will improve the success rate of implants.
|
AuthorArticles are written by Dr M Hajarat. Archives
July 2024
|
|
Niagara Park Dental
3 / 16 Washington Avenue Niagara Park, NSW 2250 Email: [email protected] Phone: (02) 4329 3003 |
HOURS
Mon 9:00 - 5:30 Tue 9:00 - 5:30 Wed 9:00 - 5:30 Thu 9:00 - 5:30 Fri 9:00 - 5:30 |
|